A Quality Life: Paul’s Ewing Sarcoma and Palliative Care Story
On good days, you can find Paul in his house intently focused on one of his woodworking projects. It’s hard work, but it’s a labor of love.
“I’m not the type to sit still. I’m at my happiest when I’m working with my hands and creating something new,” says Paul.
The fact that Paul is able to get up and do woodwork is something even he couldn’t have imagined five years ago when he was diagnosed with Ewing sarcoma—a rare cancerous tumor that grows in the bones or in the tissue around the bones. A tumor in his spine caused immense back pain, made worse by symptoms from chemotherapy, radiation, and several spinal surgeries. He couldn’t do even the smallest of tasks.
That’s when he was referred to palliative care.
Prior to the cancer diagnosis in 2012, Paul had dealt with back problems from years of working in construction. But he knew that something was different when he ended up in the hospital from a type of pain he hadn’t experienced before. When an MRI revealed he had a tumor on his spine, Paul assumed the doctors would remove the tumor and he’d be okay.
“I didn’t know it’d be quite as extensive a process,” says Paul.
The first step involved immediately starting chemotherapy and radiation, which greatly reduced the size of the tumor. In fact, Paul was ultimately cured of cancer. But severe spinal damage caused by the tumor required several spinal surgeries. He also had nerve pain in his feet and thighs, a common side effect of chemotherapy. As a result, Paul could barely walk. The physical difficulties also caused Paul to face a hard reality: he would have to leave the construction job he loved.
“My work was my identity,” explains Paul. “Having to leave that behind was very upsetting. I was in pain and I was depressed. It was hard.”
Finding Palliative Care
Sensing that Paul could benefit from better pain management and support for his emotional well-being, Paul’s oncology team referred him to palliative care.
Palliative care (pronounced pal-lee-uh-tiv) is specialized medical care for people living with a serious illness. This type of care is focused on providing relief from the symptoms and stress of serious illness. The goal is to improve quality of life for both the patient and the family. Palliative care is provided by a specially-trained team of doctors, nurses and other specialists who work together with a patient’s other doctors to provide an extra layer of support. It is appropriate at any age and at any stage in a serious illness, and it can be provided along with curative treatment.
In the initial meeting, Paul’s palliative care physician, Dr. Rab Razzak, talked to him about his goals. “I always ask my patients the same question: what brings you joy? Then it’s my job to help them take positive steps forward to regain that joy,” says Dr. Razzak.
Paul said that his ultimate goal was to become more independent and not have his life dictated by constant discomfort. He was willing to try anything to feel better.
Managing the Pain
In order to get Paul more active again, Dr. Razzak and his palliative care team reviewed Paul’s pain medications and made adjustments to find the right combination and doses to help Paul feel better with fewer side effects.
“It all comes down to communication,” says Dr. Razzak. “When we say that palliative care adds an extra layer of support, we are also talking about giving a patient more time to discuss the situation. We sit with them, talk to them constantly, and use those conversations to inform our next steps. It’s the only way to truly help the patient improve.”
The pain management process continues today, but in over two years with the palliative care team, Paul has seen results.
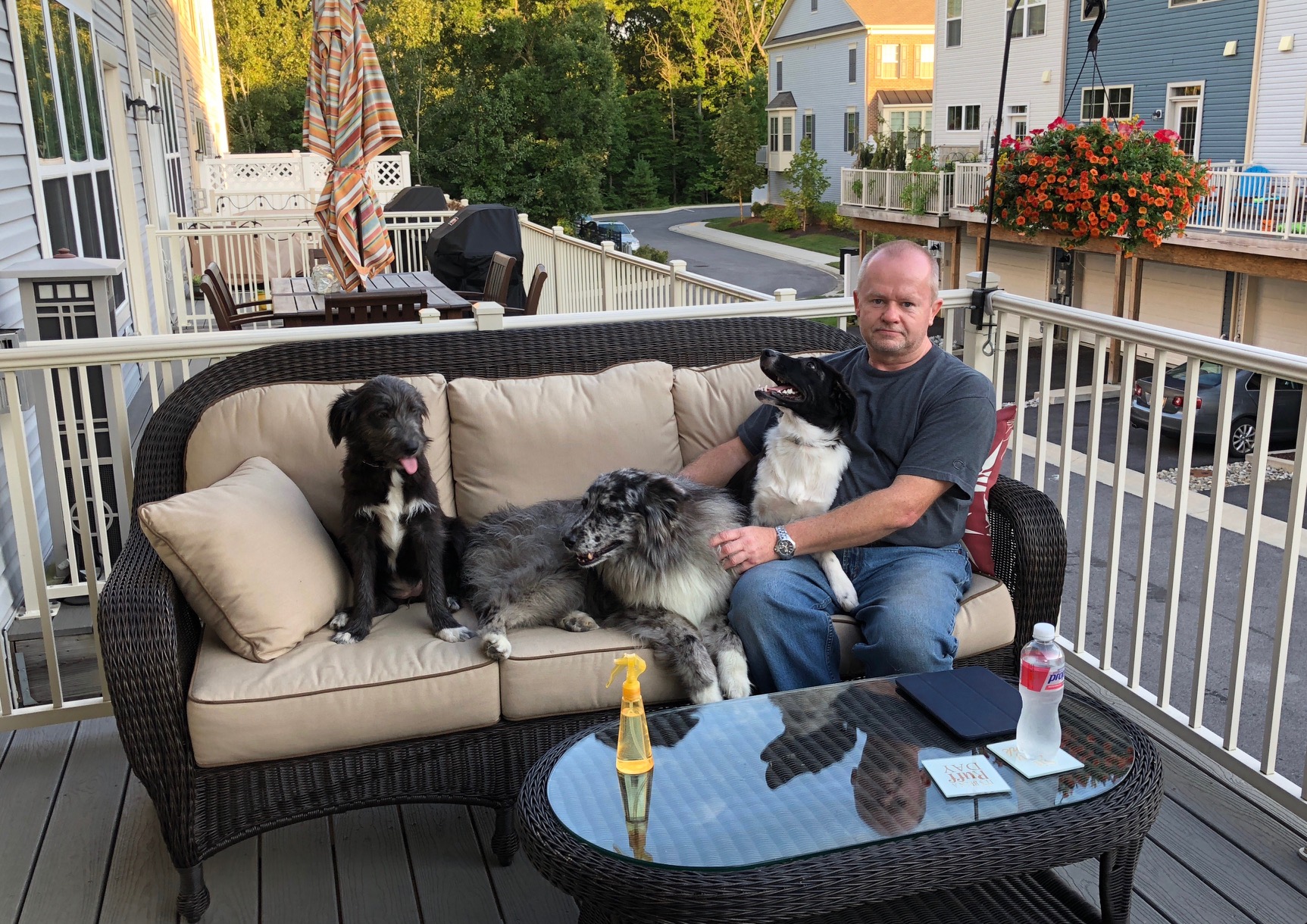
“I am finally able to live my life again. I can go out to dinner with my wife, take my dogs for a walk, and work on small projects. There are of course good days and bad days, but I can finally say that I found happiness again thanks to palliative care,” says Paul.
Paul also connects with other specialists on the palliative care team, including a social worker for emotional support and a pharmacist when he has questions about medication. The team also referred him to an acupuncturist. The result is that Paul is more active and focused on tangible goals.
Paul is ready to start a new woodworking project – making a customized pen from scratch. Just like the time it took to address his pain, he knows it will take time and effort to get the pen right.
“I’m doing well. I’m a success story,” says Paul.
To find out how you or a loved one can benefit from palliative care, visit GetPalliativeCare.Org